
In 2024, GSI began offering a Claims Tips column in the Your Plan Notes newsletters. These tips address questions from Plan Members. They are assembled here for your convenience.
Claim Tip #1: Provider Not Listed
Provider Not Listed
Professional services are a well used benefit, as indicated by the annual report from Manulife for the ELCIC Group Benefits Plan. The report showed there were 492 claimants (these could be a Plan Member, their spouse or a dependent child); as there were just over 400 active Plan Members in 2023, this averages to more than one claimant per household. Together, these claimants made 5,013 claims.
Some members have reported challenges with making a claim for professional services. The screen shot (below) shows the list to select the type of professional services provider accessed, but it is not complete.
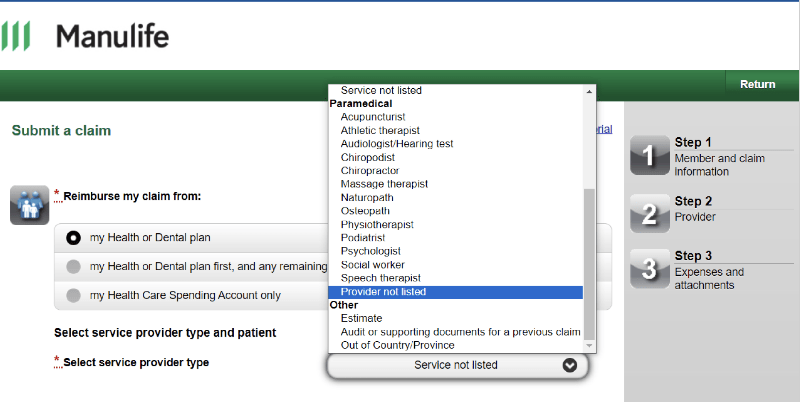 Specifically, the following providers are covered under the ELCIC Group Benefits Plan but don’t appear in the list:
Specifically, the following providers are covered under the ELCIC Group Benefits Plan but don’t appear in the list:
- Dietitian
- Kinesiologist
- Clinical Therapist
- Marriage and Family Therapist
- Master in Social Work
- Registered Social Worker
- Registered Psychotherapist
If you are making a claim for any of these, please select “provider not listed” and continue with the prompts.
Claim Tip #2: Medication when Traveling
Medication when Traveling
Standard Policy
Prescription drugs may be purchased for a limited number of days at a time:
- maintenance drugs – 100 days
- non-maintenance drugs – 34 days
 Travel plans
Travel plans
If you are travelling and your prescription refill date falls within your travel days, or if your travel is for more than 34 days, you may request an exception for certain eligible drugs.
To Apply for Exception
Call Manulife customer service at 1-800-268-6195 and provide Manulife with the exact departure and return date from your trip as well as the DIN number(s) of your medication(s).
Manulife will need 7 to 10 business days to process the request, so allow for enough time before your trip for the request to be approved and for your prescription to be filled. This is a one-time exception to for eligible drugs. Future requests if needed would will have to be re-processed.
Claim Tip #3: Dependents Traveling Alone
Dependents Traveling Alone 
Your eligible dependents are automatically covered under the travel health benefit of the ELCIC Group Benefits Plan when you enroll under any module (blue, green or teal) with family status. This coverage is valid even if they are not travelling with you.
Please note that this coverage is only available up to 60 days out-of-province or country when traveling. If your dependent is going to school, you may want to consider purchasing a student policy through the educational institution.

